The final, devastating strain of the Spanish Influenza first appeared in the third week of August in three port cities thousands of miles apart: Freetown, Sierra Leone; Brest, France; and Boston, Massachusetts. No one is quite sure how this happened:
Whether these explosions were… [the results] of a single mutation which originated in one of the three ports and almost simultaneously traveled to the other three or three different mutations will never be known. (1)
Additionally, considerable debate occurs as to whether this killer strain was actually a mutation, or just a more powerful strain naturally selected during the spring wave. Although both explanations are possible, it seems highly unlikely that the true answer will be found.
On August 27, three sailors of the Receiving Ship, a barracks for naval personnel in Boston, reported to sickbay with symptoms of influenza. By August 29, sixty-six new cases were reported. Within two weeks, two thousand cases of influenza had been recorded in the First Naval District which included the Port of Boston and the surrounding metropolitan area. On September 3, the first civilian case was reported. The deadly second wave had struck America. (2) By the end of September, 85,000 civilian cases of influenza were reported within the state of Massachusetts, and during the last week of the month, seven hundred had died. By the time the pandemic reached its peak in late October, seven hundred would die in a single day in Phliladelpha. (3)
After entering the country at Boston, the pandemic spread generally to the south and then west. International shipping brought influenza to the port cities on the Gulf of Mexico and the West coast, and this created a "pinching" effect on the Midwest. (see Figure 6)
Figure 6 — Chronological Map of the Influenza Epidemic of 1918 (4)
Within New England, influenza reached epidemic proportions by the middle of September, rapidly extending down the entire Atlantic Coast from the southern Maine to Virginia. By the first week of October, the pandemic had apparently reached all of the country except some isolated rural, Rocky Mountain states. By the third week of October, some six weeks after the outbreak in Boston, influenza had invaded every part of the country. (5)
Mortality rate statistics show that influenza's virulence appears to have dropped as the pandemic spread across the country. The maps indicate the months that certain geographic areas were first infected by the second wave (black shading), and the cities are arranged accoring to the data contained on the maps. (6)
| City | Death Rate/thousand from influenza and pneumonia (7) |
|---|---|
| Boston | 5.7 |
| Fall River (MA) | 5.5 |
| New Haven | 5.1 |
| August map | 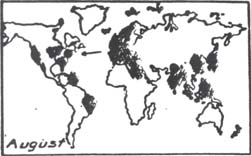 |
| Chicago | 3.5 |
| New York | 4.1 |
| Baltimore | 6.4 |
| Philadelphia | 7.4 |
| Pittsburgh | 6.3 |
| San Francisco | 4.7 |
| Los Angeles | 3.3 |
| September map |  |
| Portland | 2.7 |
| Spokane | 3.1 |
| Cleveland | 3.1 |
| Indianapolis | 2.4 |
| Seattle | 2.4 |
| St. Louis | 2.2 |
| Toledo | 2.0 |
| Milwaukee | 1.8 |
| Minneapolis | 1.8 |
| October map | 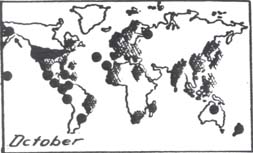 |
From these data, a general trend can be observed. The earlier in the pandemic a city was infected, the higher the mortality rate seems to be. As shown on the maps, the Northern (west of the Mississippi River) United States was the last region struck, and this region recorded the lowest mortality rates. These statistics are not surprising for like any epidemic, influenza started out very strong and slowly its potency decreased. As an epidemic progresses, the pathogenic agent infects and sometimes kills the host population attacked. If the attack does not end in death, the host can develop an immunity to that particular agent. The combination of death and acquired immunity decreases the number of hosts available to the agent. With less people to infect, the epidemic must lose its virulence.
The influenza epidemic struck the armed forces both earlier and more severely than the civilian population. In addition, because of the mobilization, i.e. the movement of thousands of men over many miles, the armed forces became, to a large extent, the source from which much of the nation contracted influenza. "The belief that the nation's protectors were now the source of its greatest immediate danger was common enough for some civilians to regard the military with fear." (8) Influenza peaked among Naval personnel on duty in the United States in the last week of September. In fact, for the first few weeks, the pandemic was mainly a naval affair. Not surprisingly, both the Navy's shore personnel and the new wave of influenza were concentrated on the East coast. Furthermore, this new wave had begun in the Navy, with their personnel significantly spreading influenza throughout the country:
On September 7, a draft of Jackies [sailors] from Boston arrived at the Philadelphia Naval Yard, where six cases of flu appeared on the eleventh. On September 17… [a] draft of hundreds from the Philadelphia Naval Yard arrived at the Pudget Sound Naval Yard in the state of Washington. Eleven were ill on arrival and the disease became epidemic in Seattle on about September 25. (9) The Navy was also responsible for spreading the epidemic to places other than seaports. In addition to Naval training detachments at colleges across the country, the Navy operated a huge inland base north of Chicago, the Great Lakes Training Station. Influenza first hit the base on September 11, and within a week, there were 2,600 reported cases. By the 20th, outbreaks were reported in Chicago's northern suburbs closest to the base, and it was a matter of days before the epidemic hit Chicago. Since Chicago was the nation's largest railcenter, the pandemic spread out in every direction. (10)
The Navy tried vainly to stop the epidemic from depleting its ranks. After a successful quarantine of the Naval Training Station on Goat Island in San Francisco Bay, in which not one case of influenza was reported, Naval Surgeons could do nothing but shrug when men released from the confinement and given liberty in San Fransisco contracted the disease. Indeed, they could not keep the men confined forever. Overall, the Navy had reported 120,000 cases, nearly one fourth of its total strength, with 5,000 dead. (11)
The Army, with approximately ten times the manpower of the Navy, suffered over 25,000 deaths in the United States. (12) The epidemic peaked among Army personnel during the week of October 11, two weeks later than in Navy. This later peak is attributed to the inland location of most army bases. The mobilized Army also spread influenza more rapidly than it would have if America was at peace. Many outbreaks throughout the Mid-West and the South can be traced to troop movements between different camps:
…influenza had spread rapidly from camp to camp, from the Atlantic seaboard to the south and west, due to the continual interchange of personnel from infected to non-infected camps. (13)
The major means of transportion was the railroad. The Army, in order to keep costs down and move the maximum number of men possible, put three men in double seats and two men in single berths (strategic packing as opposed to overloading). This crowding almost guaranteed the spread of influenza among the troops. Troops trains passed through cities and towns, and infected army personnel passed the disease on to the civilians:
The first flu appeared in Kentucky about September 29 when troops were coming through… stopped in Bowling Green, infected a few of the citizenry, got back on the train and went on their way. (14)
Soldiers and sailors were not the only carriers of influenza, only the best documented. Thousands of civilians working in the war industry crossed the the country on a regular basis. Their contribution to the spread of influenza, although not as well recorded as the military's, was undoubtedly considerable. A serviceman had easy access to free medical care, thus, military cases were more likely to be treated and recorded.
During the period of September 1st and October 31st, one out of every five soldiers stationed in the United States contracted influenza. In an effort to control the epidemic, the War Department ordered a ten percent cut in troop shipments to France, a reduction of seating on trains to one soldier per seat, and a general lowering of the intensity of training in all camps in the country. By the end of October, virtually all draft calls and training were suspended. The idea of slowing down the war effort seemed less dangerous and more sensible than trying to hold it at top speed during the pandemic. Indeed, by the first week of November, fatalities within the Army were cut in half and apparently the pandemic was losing its fury. (15)
The degree to which the armed forces contributed to the spread of influenza raises an important question: Was the magnitude of the 1918 pandemic a result of the circumstances of the times, or would it have still occurred if the world had been at peace? The answer seems to be that although the influenza virus would have been present in 1918, the circumstances of World War I perpetuated the epidemic to the killer that it became.
During 1918, there were brought together not only troops from all corners of the world, but also a large number of labourers… People were crowded together often under conditions of great misery, so circumstances were ideal for the exchange of infection and the start of an epidemic. (16)
In the United States, the war had produced ideal conditions for the spread of just such an epidemic: "Millions of people of the ages most susceptible to severe influenzal infection were jammed together in industrial cities, military camps and ships, and were shifting about… in immense numbers." (17) Once given the biological foundation, the conditions of war took over and did the rest.
Chapter III Footnotes
- Alfred Crosby, Epidemic and Peace, 1918, 1976, p. 37.
- Ibid., p. 39-40, and Hoeling, pp. 24-25.
- Crosby, p. 53.
- Ibid., p. 65.
- Warren Vaughan, Influenza: An Epidemiological Study, July, 1923, pp. 83-84.
- Ibid., p. 69.
- "Causes of Geographical Variation in the Influenza Epidemic of 1918 in the Cities of the United States," Bulletin of the National Research Council, July, 1923, p.29.
- Crosby, p. 56.
- Ibid., p. 57
- Ibid.
- A. A. Hoeling, The Great Epidemic, 1961, pp. 186-187.
- Ibid.
- Vaughan, p. 85.
- Crosby, p. 62.
- Ibid., pp. 59-62.
- William Beveridge, Influenza, The Last Great Plague, 1977, p. 42.
- June Osborn, History, Science and Politics: Influenza in America, 1977, p. 8.